Osteoarthritis: It’s Not All Doom and Gloom!
You will have all heard at some point the term ‘Osteoarthritis’, you may even have a vague idea of what it is, but for many of you that is about as far as your knowledge regarding this subject will go. Therefore this blog aims to hopefully enhance your knowledge of this troublesome condition and ensure you have a clear understanding about the what’s, whys and how’s!
What is Osteoarthritis?
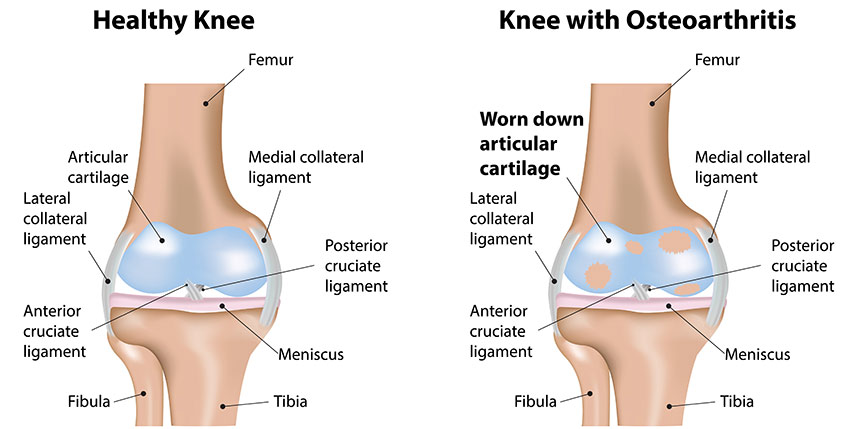
Osteoarthritis (OA) is a condition that affects the joints of our skeletal system. Although its name suggests an inflammatory background, i.e. –‘ITIS’, it is actually degenerative in nature. The phrase ‘wear and tear’ is often used and that is because this joint condition affects the bony surfaces of a joint; they become damaged causing the joint to not move as smoothly as it should. The cartilage that covers the bone ends should be shiny and smooth, when a joint develops OA this cartilage becomes pitted, thin and rough which consequently then causes the bone underneath to thicken (Felson et al., 2000).
As a result of this damage, tissues within and surrounding the joint structure will become more active changing the joints’ composition. Bony spurs will form as a result of bone growth at the edges of the joint, the ligaments and capsule (supportive structure around the joint) will gradually thicken and contract with a view to making the joint more stable, but in reality causing stiffness, and the synovium, which is the inner layer of the capsule, may also thicken and generate extra synovial fluid causing the joint to swell. In severe cases of OA, the cartilage can sometimes wear so thin that it is unable to act as a shock absorber between the bone ends and they will then actually rub against each other, causing the bones themselves to wear away. Combine this with the loss of cartilage and formation of bony spurs, your whole joint can change shape and thus force your bones out of their natural functional position.
What causes it and what symptoms you might expect
Now that you’re a bit more in tune with what OA actually is, let’s discuss what causes it and what symptoms you might expect. There are several factors that may lead to an increase in developing OA, age and gender being just a couple of them. Unfortunately, OA is more common the older we get, the reason is unknown amongst researchers but they hypothesise that it could possibly be the amount of repetition we put our joints through over the years, the weakening of muscles or even quite simply the body being less able to heal itself. It is also more prominent in females...sorry ladies! Previous joint injury can also predispose you to the onset of OA as can joint abnormalities.
It is a misconception that normal exercise will cause OA, however very hard activities that are repeated over long periods can increase your risk. Additionally, obesity is a risk factor for the development and progression of OA, particularly in the knee (Deyle et al., 2005). One thing that is overlooked is your biomechanics and how that will increase the likelihood of developing OA. Example: if you run regularly but your knee joint doesn’t move in the optimal line then it stands to reason that this will cause excessive pressure, wear and tear and overload on the cartilage and bone ends. With this in mind we believe one of the major contributing factors to OA is poor joint motion / biomechanics. So it stands to reason why age plays a role in OA. If you play any sport for a number of years with poor biomechanics its likely you will develop OA!
Pain and stiffness being the primary symptoms
Several symptoms are associated with osteoarthritis, pain and stiffness being the primary ones. It is not fully understood where the pain comes from but many believe that it is down to the degree of structural damage to the joint as well as a chronic inflammatory response associated with the debris within the joint space as a result of the degeneration to the cartilage (Girbes et al., 2013). Stiffness of the joint is felt more first thing in a morning and after periods of rest; the inactivity causes the joint and its surrounding structures to cool and therefore be much less pliable making the joint inflexible. Once up and moving around you’ll find that the stiffness eases. Swelling can also be a common symptom of OA, this can be soft in nature due to the production of extra synovial fluid or sometimes hard due to the thickening of bone. You may also feel a grinding or grating sensation on movement, again this is likely to be as a consequence of the structural damage.
What can be done about OA?
So is there anything that can be done about OA? Of course there is, unfortunately there is no way to rid you of the condition completely but there are plenty of things that can be done to reduce your pain, manage your symptoms and reduce the rate of its’ progression. Other than just relying on taking medication to ease your pain, as sports injury specialists we know that there are plenty of other modalities that can improve your symptoms and not just for the short term. The first thing is to keep mobile, within relatively pain-free parameters of course; movement of the joint helps to nourish it as well as warm it through making the surrounding structures more pliable.
You may be apprehensive to do this at first as you may experience some pain, but the more you move we promise you that the pain will ease. Loosening off and stretching the tight muscles around the affected joint will also help with restoring mobility and better function as well as helping to reduce pain (Jamtvedt et al., 2008). In addition to keeping the joint mobile, we want to strengthen it so that the muscles surrounding it can take the load rather than the joint itself. Therefore we believe strengthening exercises are essential, (Petursdottir et al., 2010) in combination with correcting your biomechanical weakness or joint mal alignment when it comes to OA. By doing so will help to prolong the life of the affected joint and at the same time reduce your symptoms…so all in all its win win!
Osteoarthritis is one of the most frequent and disabling joint pathologies in modern society affecting the older population. This degenerative condition affects the cartilage covering the bony surfaces of a joint and is likely to give rise to pain, stiffness, joint swelling and inevitably impaired function. Although irreversible, there are steps that can be taken to ensure greater manageability of OA which will aid in reducing symptoms, improving function and prolonging joint health. Keeping the affected joint mobile is key as this will reduce stiffness and pain. This in combination with a stretching and strengthening programme will help to control and minimise the rate of progression of OA and allow you to lead a normal, active life. Please don’t think that it is all doom and gloom because there are things that can be done, and here at City Rehab we really want to help!!!
Deyle, G.D., Allison, S.C., Matekel, R.L., Ryder, M.G., Stang, J.M., Gohdes, D.D., Hutton, J.P., Henderson, N.E. & Garber, N.B. (2005) Physical Therapy Treatment Effectiveness for Osteoarthritis of the Knee: A Randomised Comparison of Supervised Clinical Exercise and Manual Therapy Procedures Versus a Home Exercise Program. Physical Therapy: 85, 1301-1317
Felson, D.T., Lawrence, R.C., Dieppe, P.A., Hirsch, R., Helmick, C.G., Jordan, J.M., Kington, R.S., Lane, N.E., Nevitt, M.C., Zhang, Y., Sowers, M.F., McAlindon, T., Spector, T.D., Poole, R., Yanovski, S.Z., Ateshian, G., Sharma, L., Buckwalter, J.A., Brandt, K.D. & Fries, J.F. (2000) Osteoarthritis: New Insights. Part 1: The Disease and its Risk Factors. Annals of Internal Medicine: 133(8), 635-646
Girbes, E.L., Nijs, J., Torres-Cueco, R. & Cubas, C.L. (2013) Pain Treatment for Patients with Osteoarthritis and Central Sensitization. Physical Therapy: 93, 842-851
Jamtvedt, G., Dahm, K.T., Christie, A., Moe, R.H., Haavardsholm, E., Holm, I. & Hagen, K.B. (2008) Physical Therapy Interventions for Patients with Osteoarthritis of the Knee: An Overview of Systematic Reviews. Physical Therapy: 88, 123-136
Petursdottir, U., Arnadottir, S.A. & Halldorsdottir, S. (2010) Facilitators and Barriers to exercising Among People with Osteoarthritis: A Phenomenological Study. Physical Therapy: 90, 1014-1025

